Hemangiomas happen when developing blood vessels grow incorrectly, forming tumor-like growths. They aren’t cancerous, and they’re usually not dangerous. But when they form in the wrong place, you might need treatment to prevent complications.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
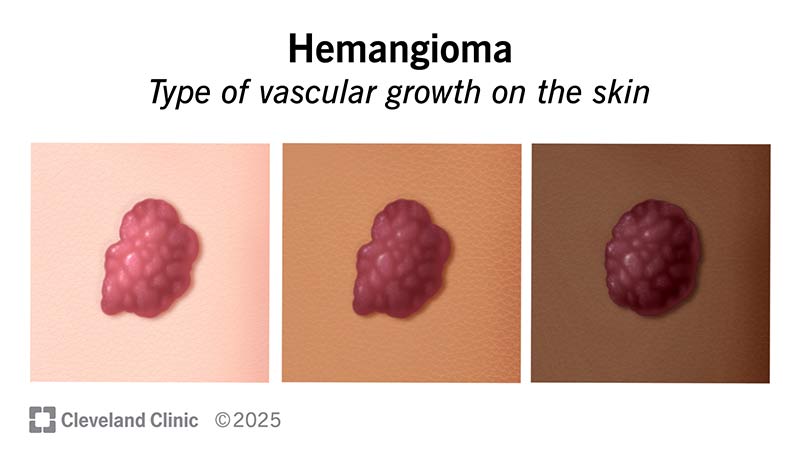
Hemangiomas are a type of growth that can appear as red or purple lumps on lighter skin or brown on darker skin. They happen when clusters of blood vessels grow and bunch together incorrectly. You can have them when you’re born, develop them during infancy or have them appear later in life.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Hemangiomas are most common in infants and children, with about 1 in 10 babies having them at birth. But adults can develop them, too. In fact, about 3 out of 4 people age 75 and older have cherry hemangiomas.
Hemangiomas are a type of benign tumor. They don’t spread to other parts of your body and aren’t cancer. It’s also extremely rare for hemangiomas to turn malignant (cancerous).
The two most common types of hemangiomas are:
Hemangiomas usually aren’t dangerous. But if they grow in a critical area, they can press on and eventually damage surrounding tissues, which can make them dangerous. How dangerous depends mainly on where exactly they are.
Hemangiomas can grow just about anywhere on your body but usually grow on your head or neck. They’re most visible when they happen on your skin. But hemangiomas can also happen on mucus membranes, like inside your mouth or on your tongue. They can also grow inside your body without you ever knowing it or having symptoms. The most common place for them to grow inside you is your liver.
Advertisement
On your skin, they can:
Hemangiomas typically don’t hurt. But they may, depending on a few factors. One of those is location. Hemangiomas may hurt if they’re large or grow in places without space to spare. Hemangiomas on your skin can also hurt if you injure them, like with a scratch or scrape. Most hemangiomas also don’t bleed without injury.
Infantile hemangiomas that develop after birth have a two-phase life cycle.
By the time involution finishes, the hemangioma is gone. Sometimes, they vanish without a trace. But in other cases, hemangiomas will leave behind scarring or skin discoloration.
Congenital hemangiomas (which you have at birth) may disappear depending on what pattern they follow. The patterns are:
Hemangiomas happen when clusters of blood vessels form and grow incorrectly. Experts aren’t sure exactly why they happen or how they form.
Several potential risk factors can make hemangiomas more likely to affect you:
Hemangiomas usually don’t cause any complications unless they grow in a critical location. Some examples include around your:
Advertisement
Hemangiomas, especially ones on your skin, often stand out. Healthcare providers may notice them during routine physical exams.
Healthcare providers can assess hemangiomas using simple devices like ultrasound. This imaging method is especially useful with hemangiomas because of the blood flowing through them. Other tests, like a biopsy to test the tissue and determine what it is, are possible but not always necessary.
In some cases, your healthcare provider might recommend additional imaging like MRI. Scans like this can help your provider check for potential risks that aren’t visible from the outside. And other tests, like blood tests or even genetic tests, may help your provider diagnose a hemangioma or rule out other conditions. Your healthcare provider can tell you more about the tests they recommend for your situation.
Hemangiomas are very treatable, but many of them don’t need it. Infantile hemangiomas commonly go away on their own, so your provider may recommend monitoring only.
Some reasons why hemangiomas might need treatment include:
Advertisement
There are a few ways to treat hemangiomas:
Cherry hemangiomas, the type that usually affects adults over 75, don’t generally need treatment. But if they’re causing issues for you, a primary care provider can refer you to a dermatologist for treatment.
You should schedule a visit to a healthcare provider if you have a hemangioma that:
Advertisement
What you can expect from a hemangioma depends on the type, where it is and when you have it. In general, hemangiomas aren’t dangerous unless they grow in certain places. And most hemangiomas will eventually shrink and fade on their own. But if your child does have a hemangioma that needs treatment, several treatment approaches are available to help.
If your child has a hemangioma and you have questions about how it might affect them, there’s someone who can help. Your child’s pediatrician can offer insight and guidance about what you can and should do to help your child. They can also reassure you and help ease your concerns.
Hemangiomas are a type of vascular birthmark, meaning they come from blood vessels. Birthmarks can be vascular or pigmented (like moles).
If your child has a hemangioma, it’s understandable to feel concerned or even worried, especially before you know what it is. And even after getting a diagnosis, the uncertainty of how it will affect them can weigh on you, too. But you don’t have to face these questions alone. Talking to your child’s pediatrician is the first step to getting answers. And their pediatrician can also reassure you and help you understand what you need to know to help your child.
Cleveland Clinic’s primary care providers offer lifelong medical care. From sinus infections and high blood pressure to preventive screening, we’re here for you.

Last reviewed on 03/28/2025.
Learn more about the Health Library and our editorial process.